SECOND OPINION SERIES
Why MTHFR Testing Fails Mental Health Patients — and Why Folic Acid Can Worsen Depression
Searches for MTHFR depression, MTHFR autism, and methylation testing for mental health have surged in recent years. Patients struggling with depression, autism, anxiety, or treatment resistance are frequently told to “check their MTHFR,” often with the implication that a single genetic result will explain their symptoms. Unfortunately, this widespread focus on MTHFR depression and MTHFR autism has led to confusion, misdirected treatment, and in many cases, worsening mental health outcomes.
A common pattern seen in clinical practice is the assumption that abnormal MTHFR results automatically justify methylfolate or folic acid supplementation. In patients with MTHFR depression, this approach can be harmful. Rather than clarifying methylation status, most methylation testing for mental health based solely on genetics fails to explain why some patients worsen instead of improving.
One of the most frequent clinical consequences of misunderstanding MTHFR depression and MTHFR autism is inappropriate use of folic acid or methylfolate. In vulnerable patients, these interventions can increase serotonin reuptake activity, reducing serotonin availability and worsening depressive symptoms—despite being prescribed with good intentions.
The Core Problem: Why MTHFR Is Not a Methylation Diagnosis
MTHFR is only one enzyme in one pathway. Mental health depends on global methylation balance, not a single genetic variant. This is the fundamental flaw in most methylation testing for mental health that relies on SNP interpretation alone.
Most genetic SNP testing used to evaluate MTHFR depression or MTHFR autism:
-
Does not measure current methylation function
-
Does not identify overmethylation
-
Does not account for opposing genetic influences
-
Does not predict how the brain will respond to methyl donors
-
Does not measure serotonin transporter (SERT) activity
Dr. Walsh describes methylation genetics as a biochemical tug-of-war, where some variants push methylation upward while others push it downward. Yet most commercial genetic panels marketed for MTHFR depression focus almost exclusively on undermethylation-related SNPs. They fail to evaluate overmethylation drivers that are highly relevant in depression and autism, making methylation testing for mental health incomplete when used in isolation.
This is why patients with MTHFR autism or depression can share similar genetic findings but respond very differently to the same supplements.
Why Folic Acid Can Worsen Depression
This is where treatment frequently goes wrong.
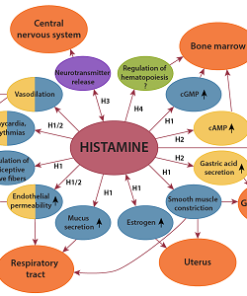
In undermethylated forms of MTHFR depression, serotonin is already being cleared too rapidly from the synapse. Dr. Walsh’s work shows that folic acid and other methyl donors can increase SERT (serotonin transporter) activity. This accelerates serotonin reuptake and reduces functional serotonin availability, directly worsening depressive symptoms.
When methyl donors are prescribed based on incomplete methylation testing for mental health, patients may experience:
-
Worsening depression
-
Increased anxiety or agitation
-
Insomnia or inner restlessness
-
Emotional flattening
-
Paradoxical reactions to SSRIs or supplements
This explains why many individuals with MTHFR depression report that methylfolate or folic acid “made them worse,” even though the recommendation was based on genetic results. The issue is not folate itself—it is giving methyl donors without understanding whether the patient is overmethylated or undermethylated.
The same risk applies to MTHFR autism, where inappropriate methylation support can increase irritability, behavioral dysregulation, or regression.
The Clinical Consequences of Misapplied MTHFR Testing
As a result of relying on incomplete methylation testing for mental health, many patients with MTHFR depression or MTHFR autism:
-
Are prescribed methylfolate or folic acid when it is inappropriate
-
Experience worsening mood, agitation, or sleep disruption
-
Fail multiple medication or supplement trials without understanding why
-
Are told the treatment “should be helping,” despite clear deterioration
This is not a failure of methylation science.
It is a failure of how MTHFR depression, MTHFR autism, and methylation testing for mental health are being applied in clinical practice—without functional biochemical confirmation.


I have the MTHFR C677T gene mutation.
I have been taking B12, methylfolate & 800 mg per day of SAMe. It worked to get some health issues cleared up.
I have done well with this treatment for several years but have recently developed constant diarrhea which I have had for 3 mos. Nothing seems to help. I’m currently on medical leave from teaching. I also have always had high levels of inflammation in my gut, allergies & food sensitivities. Help! I have lost over 15 lbs and did not have much weight anyway, being a competitive distance runner athlete. I’m not doing much exercise lately which may contribute to issue. Have taking care of aging parents. They are doing better than me! Some family members have had bouts w depression. I’m doing ok in that aspect.
Any suggestions that might help me to clear up diarrhea?
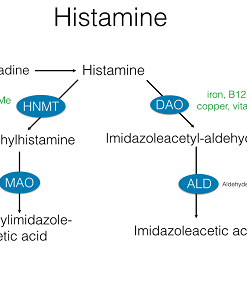
Hi Linda, SAMe and folate have opposing effects on serotonin and dopamine activity. Suggest testing histamine levels to determine status of methylation before taking either of these supplements.
What test do you run to check histamine levels
And
What about whole blood histamine to determine methylation status?
Whole blood histamine is ordered to determine methylation status. Typically this is ordered with homocysteine in order to determine best supplement plan.
My gf is bipolar and we started the Walsh nutrient therapy 3 months ago. She is undermethlated with a slight copper overload. We did the blood test to determine these results with a nuturalpath who does the Walsh protocol. She has had three psychosis breaks since Jan 2018 and each resulted in hospitalization. She is taking 80mg of latuda at supper, 1200mg of lithium and 15mg of olanzapean at night. The nutrient protocol recommendations are 10,000IU vitamin A, P5P, Vitamin E, liposimol Glutithione, Sam-e, Zinc. Her has
Complained about stomach upset for months
And still has some psychotic thoughts such a spirits and demons needing to be fought. Can I do more the help with her stomach and brain functions now that we know she is under methylated? I’m thinking shamanic healer for emotional trauma in conjunction with psychologist and olive leaf with a probiotic? She wants to lose weight and has had a very difficult time doing that.
What you describe is not a full protocol for undermethylators. Further complicating the issue are these medications. I suggest you coordinate with the Walsh Practitioner and your prescribing physician to determine if medicine levels can or should be adjusted. Before changing doseages of medications or supplements it would be helpful to see how the labs and symptoms have changed, if at all, since she has started supplementation.
Hello . I m from india . First i dignosed with ocd , sexual obsessions . Got 150mg sertaline and aripiprazole 5 mg . Took 4 years . I thought i m ok with these medicines but it was hypomania . I realized and stopped medicines . Then i got bipolar 2 dignosis . No lithium lamictal worked for me . Just made me more depressed . I tried vitamin minerals then but nothing working . My folate level is 0.8 and b12is 238. What should i do . Plz tell.
Folates are not recommended for persons who are depressed or with similar symptoms unless a whole blood histamine test or methylation panel has definitively shown that one is OVERmethylated. We do not use folates in undermethylated persons because it acts on the reuptake protein production, lowering production and thereby increasing reuptake, which is good for overmethylators, who have high levels of serotonin and low folates.
This article currently states that 18 percent of depressed patients are overmethylators with low serotonin and dopamine. I believe this should say elevated levels of serotonin and dopamine with low levels of histamine.
Thank you for spotting that typo.
I had a minor surgery 3 years ago and woke up in a state of panic and felt like nothing was real for about 7 days. When the acute episode ended I started becoming depressed, suffered from chronic anxiety and panic attacks daily, i took a pediatric dose of xanax just so I didn’t feel like I was dying 24/7. I eat very well, am a whole foods nutritionist but nothing worked naturally. I thought I was loosing my mind. I finally started zoloft and after 2-3 months it started to work. For 2.5 years I was fine and I was titrating off the whole time because I felt normal again, I had a history of anxiety but kept it in check for 20 years with diet and exercise, absolutely no medication. So I thought that 3 months was just an episode, I had recently moved 1000 miles away from any family with 3 children, just had my 3rd when it happened and I was lowered to 25 mg then 15 mg of zoloft over the course of a year . When I finally stopped the zoloft all of the symptoms reappeared. I tried everything, exercise, a host of natural supplements, b vitamins, rhodiola, ashwaganda, mag taurate but nothing worked and I was again in the same state. I am now on 50 mg of zoloft and feeling better but I went to a functional medical doctor and had extensive testing done. No smoking gun, my protein was low, some viral concerns and inflammation and my kidneys were not doing that well but everything else was fine, my B vitamins, vit D, my hormones. I want off this medication because I know it is not correcting the real issue but I am so afraid to go through that again. This doctor says he is going to work on methylation and my neurotransmitters. It is going to cost 4-5 thousand dollars and I just feel so defeated.
The history is relevant in order to determine symptoms, medication history and past results. However, to get a good idea of the biochemistry associated with neurotransmitter levels a Walsh-trained physician and a Biotype blood panel should provide actionable information.
I am definitely high in histamine, and low in neurotransmitters. I am an undermethylator. My test results came back high in methyl-histamine; I have all the symptoms of an undermethylator (ie…previous diagnosis of Interstial cystitis that went away after time, flusing, itching skin when I run, anxiety, racing thoughts, etc…… However, when I try to supplement such as SAMe or 5HTP, I get very nauseous and wired. I am already wired from being undermethylated and can’t take more anxiety from SAMe and Nausea from 5 HTP. What other supplements should one take if the suggested supplements for an undermethylator make him/her wired and nauseous? Is this common?
It is important when treating elevated histamine to know copper/free copper status, vitamin D levels and to know one’s homocysteine levels and cardiac risk factors. Treating with SAMe or methionine is not a complete methylation program and may cause problems if other issues are not addressed first. Best to start a treatment plan with these possible issues addressed. Once corrected, if imbalanced, it is easier to handle SAMe and methionine. Nausea is common with digestive inflammation, yeast and leaky gut. 5HTP is not part of our protocol even with undermethylators.
17 year old son, recently diagnosed with depression, OCD. He hid it for several months, until suicidal ideation became a factor & he informed us. We immediately sought treatment via psychological & psychiatric avenues. Evaluation recommendations include weekly counseling sessions & medication (currently 2mg/day Abilify for past 2weeks). I’ve insisted on getting to the root cause, which is a slow, painful process. So far only managed to get MTHFR test (no abnormality there) & neurotransmitter panel, which showed elevated histamine, yet normal to slightly high serotonin, dopamine & norepinephrine. However, epinephrine & PEA were low. Began supplementation, before getting testing, with magnesium (insomnia), D3, C, multivitamin, B complex, inositol, & fish oil. Within last 2weeks, per Dr. recommendation, added adrenal support, benedryl, phenelyalanine & Abilify. His mood has seemingly improved in the last week 1/2. I still want to get to the root issue, as I believe depression is a symptom & not a diagnosis, & wonder what further testing is recommended, as I have to push to get it done. Also regarding methylation status, he has conflicting symptoms. So, I’m trying to determine cause of histamine elevation(allergy, stress, dehydration, etc…) & should I be more concerned with why it’s not being broken down. Also, benedryl? He exhibits no allergy symptoms. Sorry, this is so long, I’m trying so hard to advocate for my son & get him well & happy again. Any advice would be greatly appreciated. Thank you.
There are a number of conflicting strategies here. While histamine is a co-factor in depression, it is not likely the cause. MTHFR does not tell us much about methylation status, nor should it be a recipe for supplementation. Suggest the methylation panel of histamine/homocysteine – this will tell us if your histamine is elevated due to undermethylation. Supplements that improve methylation, sans folates, will be best if your whole blood histamine is elevated.
Hi! Could you explain why neurotransmitter precursors such as tryptophan/5-HTP or Tyrosine/Phenylalanine are not mentioned in your protocols? Undermethylators are said to be low on neurotransmitters and it would seem like they could only help in their production. Is it OK to take them?
As Walsh describes in his physician trainings, the issue is not with insufficient levels of neurotransmitters; the issue is with reduced activity. With undermethylation the problem is due to an excessive expression of SERT and DERT neurotransmitter reuptake promoters. Excessive reuptake is why SSRI drugs, reuptake inhibiters have become the main focus of antidepressant medicine research and therapy. When we thought diminished levels of neurotransmitters were the issue, the treatment was MAO inhibitors; this is no longer the desired approach.
Yes, that’s a great questions. We don’t useS serotonin precursors in the Walsh approach for a similar reason that pharmaceutical MAO inhibitors are used less often these days than SSRI drugs. The production levels are less important than the activity or reuptake activity of the neurotransmitters. Methylation is important with regards to serotonin activity from the epigenetic influence it has on the DNA that transcribes serotonin reuptake transport proteins. Undermethylators produce a high amount of these reuptake proteins, which lowers the effectiveness of the neurotransmitters. Most undermethylators respond better to methylation for its epigenetic influence on increasing methionine or methyl groups that act on the DNA.
My daughter got her period less than a month ago and immediately started experience intruding/racing thoughts and severe anxiety. This has been going on for three weeks with very little relief. What is your recommended course of action at this point. Do you have any recommendations for someone to run comprehensive blood work to see what supplements and nutrients will give her some relief? We are in San Antonio TX. Thank you!
Hi Ana, I’m sorry to hear about your daughters condition. Hormone changes frequently lead to mood disorders due to the Biotype Dr Walsh refers to as “copper overload.” Combined with low vitamin D and or elevated whole blood histamine, this is a very common cause for intruding thougths and severe anxiety. Depending on urgency you may want to see a local physician and have her evaluated to be sure she is not in any danger. If not so urgent, I would consider test Copper Overload Biotype, Histamine and Vitamin D levels. In case you would like my assistance with lab selection and assessment of results, I am following up with an email to introduce you to the protocol.
Sorry for the delayed reply. I was not aware of this message. Severe anxiety with menstrual changes may be due to estrogen and copper imbalance. The Comprehensive Biotype panel will help determine copper overload status as well as methylation and other factors such as Vitamin D levels. This is the best place to start.
Hello,
i would please like to ask a question about what happens in the case that someone, due to homozygous C677T MTHFR, has very Low Folate in blood tests, and also has high homocysteine in blood tests. The normal response would be to take more folate to correct the folate deficiency and also to lower the high homocysteine. But, what happens if this person is also an undermethylator? This would be something of a paradox, because this person should take more folate to correct the folate deficiency and lower the high homocysteine, but the extra folate would cause him/her to have what dr. walsh says a serotonin reuptake promotion so there would be a worsening of this person’s existing psychological symptoms (depression/anxiety or ocd). What should happen in such a case as regards to supplements? And also shouldn’t such a person avoid SAMe, because it would make the homocysteine rise even more?
Thank You
These are all good questions. Folate tests serum or blood are not reliable or else expensive. Values fluctuate and testing is not consistent. Homocysteine, homozygous SNPs and RBC morphology are helpful to determine but Walsh’s research indicates that most who are genuinely undermethylated (elevated WB Histamine) are not folate deficient. Most often it is the overmethylator who is and they frequently have the macrocytosis to confirm. I suggest determining methylation status with a whole blood histamine level and make a folate assumption based on that plus CBC and homocysteine. Chronic folate deficiency is reflected by an almost certain macrocytosis, as long as B12 deficiency is ruled out. Folate should be taken when levels are low and plus macrocytosis with normal B12, plus elevated homocysteine and/or when planning conception. FYI, homocysteine may be lowered with TMG, serine, B6 and NAC – it’s not just about B12 and folate or the genetic SNPs. If an undermethylator is with MTHFR / C6771, plus macrocytosis and low folate, then a low dose of folic acid, if it doesn’t significantly worsen a bad case of depression, may be tolerated and necessary. There are a lot of ifs and what ifs because there are many functions that biochemistry performs in the body and people have unique variables. Get a WB Histamine, CBC and homocysteine, plus a Walsh trained doc to review your history. And start slowly. Nutrients are much more forgiving than pharmaceuticals.
Hi,
I have been very depressed and anxious for as long as I can remember. I started a new supplement today, folinic acid. I can hardly put into words how great I feel, I hope this continues to work for me. I feel like a totally different person, the horrible black cloud has lifted. I am hoping that this bit of info can be helpful to others who are suffering as I have. God bless and don’t ever give up.
Please be careful supplementing with folates. Most people do well when depressed for the first few days but a signifiant number then notice a worsening of mood related symptoms. The reason is that it will quickly increase methylation but then it acts on the reuptake of serotonin to decrease the activity of serotonin. This is more pronounced than the increase in production of serotonin from improved methylation. Suggest testing whole blood histamine to know what is your actual methylation status prior to taking folates, niacin, choline and dmae.
This is Sandy again, from 1-10-20 post. You were absolutely correct, the wonderful feeling only lasted three days. Yesterday I woke up feeling like a truck had run over me, depressed, and had a horrific headache that lasted all day. Having those wonderful three days has given me a glimpse of how my future could look, the happy-go-lucky gal is fighting to get out. I have made an appointment for consultation with you and am excited about talking to someone who understands this yucky condition.
Hi Sandy, Thanks for your feedback. You have experienced the difficulty of taking folic acid for a mood disturbance without first ascertaining methylation status. Your response demonstrates why so many others do poorly by taking multi vitamins and b-complex when depressed, prior to utilizing histamine as a measure of true methylation status. Typically folates, niacin and DMAE are restricted to overmethylators (low WB histamine), those with high homocysteine (non responsive to B6, and B12), macrocytosis (non responsive to B12), and low serum folate levels with homozygous methyl enzyme genetic SNPs.
I’ve struggled with leaky gut lately, and have been on a strict anti-inflammatory diet with low carbs since november, along with olive leaf and other antifungals. I have been taking multivit, C-vit, E-vit, and then added B-complex in january. Since january my histamine intolerance (which I didn’t have before november) has gone sky-high, and I have become very sensitive. Since january I have also been struggling with stress, anxiety and depression. My folate level was slightly elevated before I started B-complex.
I have now stopped B-complex and multivit due to folate. I believe this indicates I am under-methylating?
I was considering starting SAM-e. But should I do ant tests first?
Yes, the test is important. Plasma histamine and symptoms related to histamine intolerance do not always imply someone has high Whole Blood Histamine. Treating incorrectly can have the opposite of a desired effect. That can be particularly deleterious with depression, schizophrenia, psychosis and other mood disorders.
I’m an undermethylator, depressed and homozygous C677T. My homocysteine levels aren’t fine. 5-MYHF, folinic acid, Folate, B’s and multiplied vitamins often make me feel worse. What would you recommend I take?
Take the Whole Blood Histamine test. Best to know for sure if you are an undermethylator. Genetic testing does not provide that information. It may show a defect in one or two of many genes that influence methylation but a better test is the WB Histamine or the Doctors Data Methylation Panel.
Methylating supplements besides folate, would include SAMe and methionine, plus magnesium, trimethylglycine and maybe supplements that help convert methionine to SAMe, such as CoQ10 and other mitochondrial support. Best to look at plasma methylation panel first to know what exactly is going on with the methylation pathway. This is much more useful than genetic tests.
I would like to know if my daughter is undermethylated or overmethylated. She had a breakdown in 2013 and had to be hospitalized. She lost over 15 pounds on a small body frame, which I think helped with the physchosis. In the hospital they put her on halpidol, seroquil, depakote and different medications for physchosis and bipoplar disorder. Since, she has continued on and off using seroquil and depakote, but keeps experiencing depressive moods, with negative thougts and beliefs. Can you help with what supplements and vitamins, food natural remedies will help to get off this horrible medication.
Yes. The goal with biochemical evaluation and use of supplements is to help patients recover from mood disorders and get off of all medications. The first step is to do the Comprehensive Biotype Lab Panel and complete a questionnaire for evaluation. Then the process of supplementation begins. After some weeks, when mood has stabilized we then consider working with prescribing physician or primary doctor to ween off medicines.
The best place to start is with whole blood histamine. The medicines may make this test ambiguous, but it is still possible to rule out overmethylation. If that is unclear, the plasma methylation panel, by Doctors Data is best.