Female Hormone Panel – Hirsuitism Evaluation
$180.00
Total and Free Testosterone
Sex Hormone Binding Globulin
Prolactin
TSH
DHEA-S
17-OH Progesterone (serum)
LH and FSH Hormones for LH/FSH Ratio
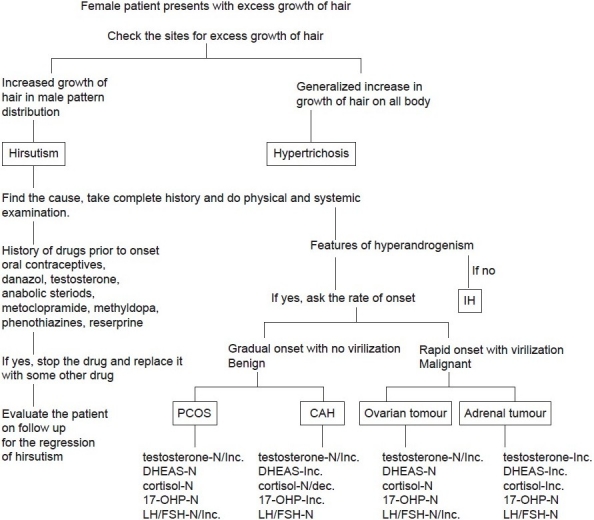
Classically, hirsutism has been considered a marker of increased androgen levels in females from increased production of androgens (i.e testosterone) either by the adrenals or due to an ovarian disease.[4,5]
The ovarian causes for hyperandrogenism are polycystic ovarian syndrome (PCOS) and ovarian tumors. Adrenal causes include Cushing’s syndrome, androgen-producing tumors, and congenital adrenal hyperplasia (CAH), most commonly due to 21-hydroxylase deficiency. Less common causes include the hyperandrogenic-insulin resistant-acanthosis nigricans syndrome (HAIRAN). Hyperprolactinemia by increasing adrenal dihydroepiandrosterone sulfate (DHEA-S) production may cause hirsutism. Androgenic drugs are also an important cause of hirsutism[6] [Figure 1]. About 20% of the patients may present with idiopathic hirsutism (IH) with normal androgen levels and ovarian function. The cause of increased hair in these women is thought to be related to disorders in peripheral androgen activity.[7] Onset of IH occurs shortly after puberty with slow progression. PCOS and IH account for 90% of the hirstutism in women. Hirsutism can also occur in some premenopausal women and continue for a few years after menopause. This is due to decrease in ovarian estrogen secretion with continuous androgen production.[8]
This is a fasting test panel and includes:
Total and Free Testosterone; (CPT# 84402, 84403, LC 070085)
Sex Hormone Binding Globulin (CPT# 84270, LC 082016)
Prolactin (CPT#84146, LC004465)
TSH (CPT# 84443, LC 004259))
DHEA-S (AM) (CPT#82627, LC 004020)
17-OH Progesterone (this should be done between 7-9am on days 1-5 following the starting day menstruation) (CPT#83498, LC 070085)
LH and FSH Hormones (for LH/FSH Ratio) (CPTs# 83001, 83002, LC 028480)
Detailed history incuding age of onset (puberty, middle age, menopause), rate of onset of symptoms (gradual or sudden), any signs or symptoms of virilisation (acne, deepening of voice, infrequent mensturation, loss of breast tissue or loss of normal female body contour, clitoromegaly, increased libido, increased muscle mass as in shoulder girdle, malodorous perspiration etc), history of weight gain or diabetes and drug history prior to onset should be taken.When a female patient presents with the chief complaint of increased growth of hair, it is imperative to see whether the coarse hairs are localized in male distribution or there is generalized increase in growth of the hair on all of the body (hypertrichosis).[9,10] After determining hirsutism, the follwing steps can be undertaken to find the cause [Figure 1].
-
Complete general physical and systemic examination should be done including palpation of abdomen for any ovarian mass.
-
If drug is the cause, simple withdrawal of the drug should be helpful. For all other cases, laboratory evaluation of the serum markers to know the exact etiology should be done. The various serum markers are-
-
Testosterone – Serum testosterone may be normal to increased in case of benign pathology as PCOS and CAH but would be definitely raised (>200 ng/ml) in case of malignant tumor of the adrenal or ovary.[11]
-
Dehydroepiandrosterone sulfate (DHEAS) – Raised DHEAS (>700 μg/dl) always indicates an adrenal cause, benign or malignant.
-
17 Hydroxy progesterone – This serum marker is unique for congenital adrenal hyperplasia. The measurement should be done between 0700 and 0900 hours in the early follicular phase of the menstrual cycle. Levels less than 200 ng/dl excludes the disease. Mildly increased levels between 300 and 1,000 ng/dl require an ACTH stimulation test. Cosyntropin (synthetic ACTH), 250 μg, is administered intravenously, and levels of 17-hydroxyprogesterone are measured before and one hour after the injection. Post-stimulation values (>1,000 ng/dl) constitute a positive test.[11]
-
Twenty four hour urine free cortisol should be measured in women with signs and symptoms of Cushing’s syndrome.
-
LH/FSH greater than 3 is indicative of PCOS.[12]
-
Prolactin would be raised in hyperprolactinemia due to hypothalamic disease or a pituitary tumor.
-
Serum TSH: Hypophyseal hypothyroidism[13] can act as a cofactor in hirsutism causing raised TSH.
-
-
Pelvic ultrasonography can be done to detect an ovarian neoplasm or a polycystic ovary.
-
Magnetic resonance imaging (MRI) or computed tomography (CT) of the adrenal region is useful for diagnosis.