Vitamin D, 25-Hydroxyvitamin D (Calcifediol)
$35.00
Vitamin D #82306
Vitamin D | Calcifediol |25 dihydroxy vitamin D
Interviewer: Dr. John Campbell
Dr. John Campbell is known for his educational content on health, nursing, and science topics, particularly on platforms like YouTube. He holds a PhD in nursing and health sciences and has a background in teaching and research in higher education. His work often involves analyzing current health studies, public health policies, and providing insights into various health-related issues, including the COVID-19 pandemic. His approachable style and ability to break down complex medical information into understandable content have earned him a wide audience. While he is not a medical doctor, his expertise lies in his analysis and discussion of peer review published research.
Interviewee: Dr. David Grimes
Dr. David Grimes is a retired consultant physician with a long-standing career in gastroenterology and general internal medicine. He has published extensively on Vitamin D and its implications for human health beyond bone metabolism, including its effects on immunity, chronic disease prevention, and its potential role in mitigating complications from infections like COVID-19. Dr. Grimes has been a vocal advocate for recognizing the broader health benefits of Vitamin D and the need for higher supplementation doses than currently recommended by many health authorities. His expertise is based on years of clinical practice, research, and a critical review of the literature concerning Vitamin D's role in health and disease.
Their discussion bridges practical clinical experience and a thorough review of scientific literature, aiming to shed light on the nuances of Vitamin D supplementation and its potential impact on public health.
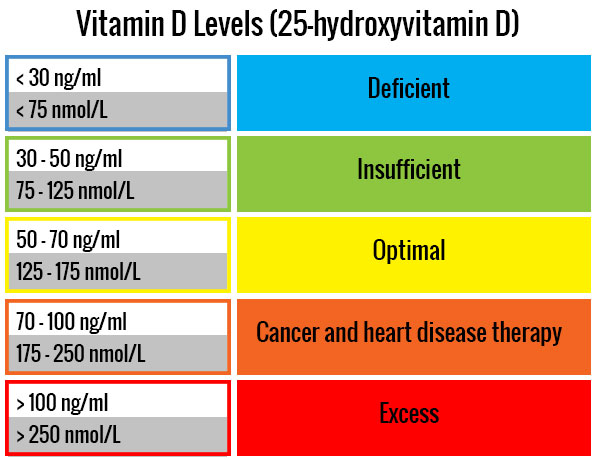
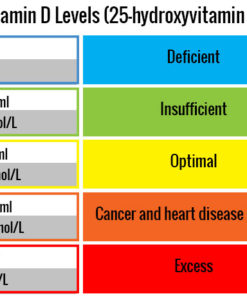
- Need for Testing: A controversial point is the need for regular blood level testing of Vitamin D. Dr. Grimes advocates for testing to ensure individuals reach a blood level of Vitamin D considered protective against infections and chronic diseases (100-150 nanomoles per liter). However, routine testing is not widely practiced or recommended by all health authorities, leading to a lack of standardized approaches to Vitamin D supplementation and monitoring.
- Dosage: One of the most debated aspects is the appropriate dosage of Vitamin D for optimal health benefits. While some recommendations suggest a modest intake of around 400 units daily to prevent conditions like rickets, Dr. Grimes argues for much higher doses (up to 6,000 units daily for an average adult) to maintain immunity and overall health. This discrepancy in dosage recommendations stems from differing interpretations of Vitamin D's role beyond bone health, including its impact on immunity and chronic disease prevention. Overdose is rare. Calcium is not required when taking vitamin D. In fact, vitamin D removes the need for calcium supplementation.
- Benefits Beyond Bone Health: Vitamin has proven to be effective reducing the risk of infections like influenza and COVID-19, chronic diseases such as certain cancers, and autoimmune conditions. The role of Vitamin D in modulating the immune response, especially in reducing inflammation and enhancing the body's defense against pathogens, is highlighted as a significant area of interest and debate.
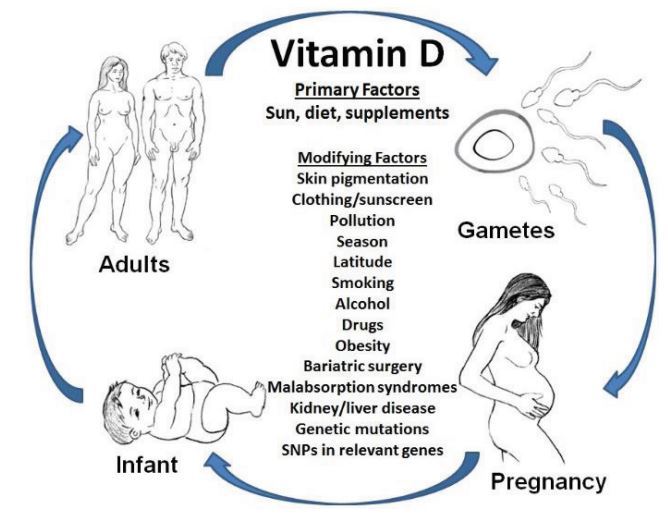
- Optimal Levels for Different Populations: The discussion touches on how optimal Vitamin D levels might vary among individuals based on factors like body weight, age, and skin color. The need for higher doses in certain populations, such as obese individuals or those with darker skin living in less sunny climates, underscores the complexity of establishing universal dosage recommendations.
- Vitamin D Deficiency in Healthcare Settings: Dr. Grimes points out a critical gap in healthcare practice regarding the management of Vitamin D deficiency, especially in acute settings like hospitals and during the pre- and post-operative periods. The potential benefits of administering active forms of Vitamin D to rapidly improve immune function in patients with infections or undergoing surgery is presented as an underutilized intervention.
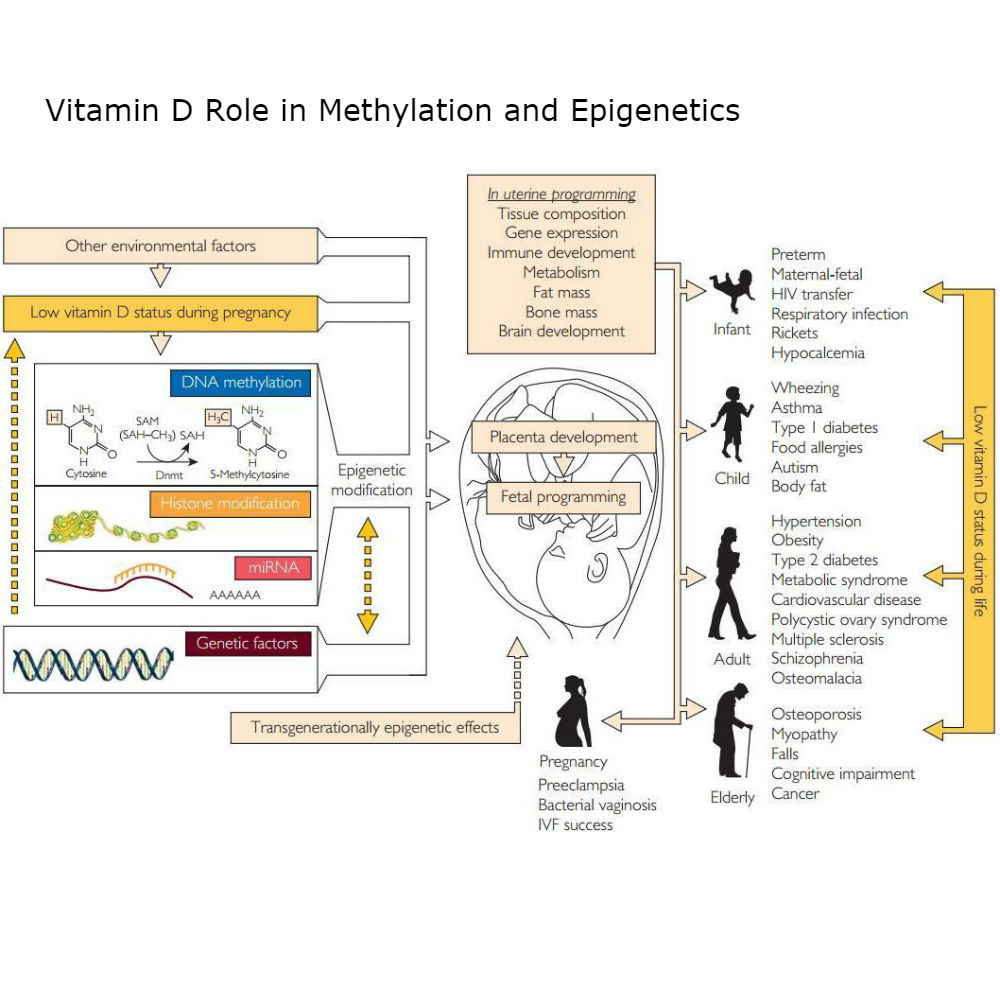
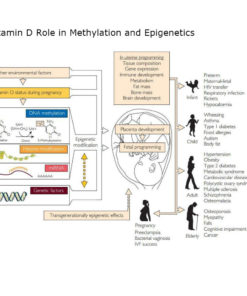
Effect of Vitamin D on Methylation and Serotonin Receptor Sensitivity
Association of Low Vitamin D Methylation of DNA:
Vitamin D has been implicated in the regulation of epigenetic events, including DNA methylation. DNA methylation is a process that controls gene expression and can be influenced by various factors, including nutrition and exposure to certain environmental conditions.
Research has shown that vitamin D can affect DNA methylation patterns, particularly within genes associated with autoimmune diseases, cancers, and cardiovascular diseases. It is postulated that vitamin D influences the methylation process through the vitamin D receptor (VDR), which interacts with enzymes responsible for adding or removing methyl groups to the DNA molecule. However, the specific mechanisms and outcomes of these interactions are complex and not yet fully understood. Deficiency in vitamin D might affect normal methylation patterns, potentially contributing to disease development.
Vitamin D and Serotonin Receptor Activity:
Serotonin, a key neurotransmitter, plays an essential role in numerous biological processes, including mood regulation, social behavior, appetite, digestion, sleep, and memory. Vitamin D appears to influence serotonin synthesis and signal transduction.
Vitamin D can influence the production of serotonin by regulating the expression of tryptophan hydroxylase 2 (TPH2), an enzyme involved in the synthesis of serotonin in the brain. When vitamin D binds to its receptor (VDR), it may promote the transcription of the gene for TPH2, thereby increasing the synthesis of serotonin.
Furthermore, vitamin D might play a role in the function of serotonin receptors. Some research suggests that vitamin D may help to upregulate serotonin receptor expression and enhance serotonin-mediated responses, though more research is needed to fully understand these mechanisms.
The relationship between vitamin D, DNA methylation, and serotonin receptor activity underscores the complexity of vitamin D's roles in the body and its potential relevance to conditions like depression, schizophrenia, cardiovascular disease, and certain cancers. It's important to note, though, that while these relationships are supported by some research, they are still areas of active study and not yet fully understood.
Why Doctors Recommend Ordering Calcifediol vs Calcitriol:
When testing for vitamin D levels in the body, healthcare providers typically measure the amount of 25-hydroxyvitamin D, also known as calcifediol, rather than 1,25-dihydroxyvitamin D or calcitriol, the active form of the vitamin. This is due to several reasons:
- Higher Concentration: Calcifediol is present in the blood at higher concentrations than calcitriol.
- Longer Half-Life: Calcifediol has a longer half-life in the body than calcitriol (approximately 2 weeks compared to 4 to 6 hours for calcitriol). Therefore, calcifediol levels provide a more stable and accurate reflection of vitamin D status over time.
- Regulatory Mechanisms: The kidneys tightly control the conversion of calcifediol to calcitriol as part of the body's regulation of calcium and phosphorus. Even if a person is deficient in vitamin D, their calcitriol levels could be normal or even elevated due to these regulatory mechanisms. Therefore, calcitriol levels are not a reliable indicator of total body vitamin D status.
It's important to note that while measuring calcifediol is the standard method of assessing vitamin D status, it does not provide a measure of all aspects of vitamin D health, such as its conversion to its active form or its effects on cellular signaling and gene expression. Therefore, a comprehensive evaluation of a person's health and other tests might be necessary for a complete understanding of a person's health status.
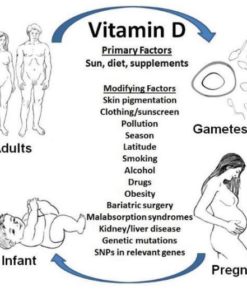
Causes of Vitamin D Deficiency
Limited Exposure to Sunlight:
- Due to lifestyle (indoors most of the time, wearing clothing that covers most of the skin)
- Living in northern latitudes where there is less sun exposure, especially in winter.
- Using sunscreen, which blocks the sun's rays that the skin needs to produce vitamin D.
Dietary Factors:
- Following a strict vegan diet. Most natural sources of vitamin D are animal-based.
- Malabsorption issues due to conditions like celiac disease, Crohn’s disease, and cystic fibrosis, which affect the intestine's ability to absorb fat (vitamin D is a fat-soluble vitamin).
Health Conditions:
- Obesity: Fat cells extract vitamin D from the blood, altering its release into circulation.
- Kidney and liver diseases: These conditions can affect the ability to convert vitamin D into its active form.
- Hyperparathyroidism: Overactive parathyroid glands can cause excessive calcium absorption, which can result in vitamin D deficiency.
Age:
- Older people have thinner skin, which may result in less vitamin D being produced when they're exposed to sunlight.
- The ability to convert vitamin D into its active form decreases with age.
Genetics:
- Variations in genes related to vitamin D metabolism (e.g., GC genes, which produce a vitamin D-binding protein, or CYP2R1, CYP27B1, and CYP24A1 genes, which are involved in the conversion of vitamin D into its active form).
Other Factors:
- Certain medications can alter vitamin D metabolism, such as anticonvulsants, glucocorticoids, antifungals, and HIV/AIDS medicines.
- Infections, especially those that result in prolonged inflammation, might influence vitamin D status. Chronic infections could lead to lower vitamin D levels due to increased inflammation and metabolic demand.
- Chronic stress and high cortisol levels may also potentially impact vitamin D levels
Vitamin D Deficiency and Treatment Options
- Symptoms of Deficiency: Symptoms can include fatigue, bone pain, muscle weakness, mood changes, and frequent illness.
- Treatment: Treatment typically involves increasing sun exposure, altering diet, or taking supplements. Dosages will depend on the severity of the deficiency, age, weight, and other individual factors.