Comprehensive Stool Analysis + Parasitology (Doctors Data)
$405.00
CPT# CDSA-A
Comprehensive Stool Analysis + Parasitology
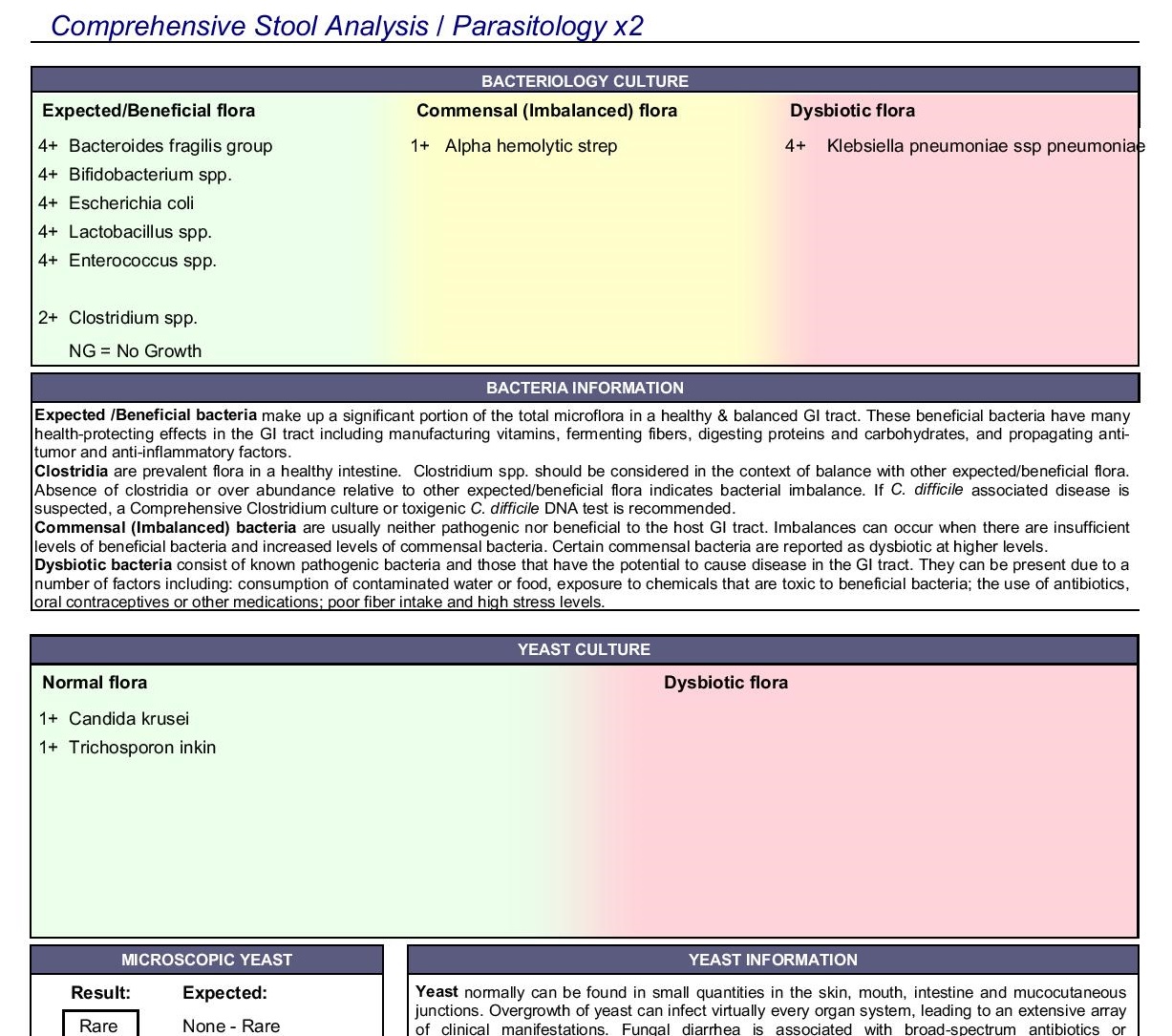
Gastrointestinal complaints are among the most common in medical care. The CSAP profile helps pinpoint the causes of gastrointestinal symptoms and chronic systemic conditions, and measures key markers of digestion, absorption and inflammation. It contains comprehensive bacteriology and yeast cultures to identify the presence of beneficial flora, imbalanced flora including Clostridium species, and dysbiotic flora, as well as the detection of infectious pathogens and parasites by PCR and other gold standard methods. Antimicrobial susceptibility testing to prescriptive and natural agents is also performed for appropriate cultured bacterial and fungal species at no additional charge. Parasitology testing can include one-, two- or three-day collection, based on practitioner preference.
Useful for:
- Gastrointestinal Symptoms
- Autoimmune Disease
- IBD/IBS
- Inflammation
- Food Sensitivities
- Nutritional Deficiencies
- Joint Pain
Turnaround Time
6 to 8 days
Note: Turnaround times on results are an estimate and are not guaranteed. The lab may need additional time due to holidays, confirmation/repeat testing, etc. You can contact us to discuss when your results should be ready.
Analytes Tested
Click any analyte name for additional clinical information, including reference ranges, specimen collection, stability and rejection criteria.
| Total List Price | $637.00 | ||
Detailed Information
The Comprehensive Stool Analysis + Parasitology (CSAP) is an invaluable non-invasive diagnostic assessment that permits practitioners to objectively evaluate the status of beneficial and imbalanced commensal bacteria, pathogenic bacteria, yeast/fungus and parasites by culture, PCR, and other gold standard methods.. Precise identification of pathogenic species and susceptibility testing greatly facilitates selection of the most appropriate pharmaceutical or natural treatment agents.
Inflammation can significantly increase intestinal permeability and compromise assimilation of nutrients. The extent of inflammation, whether caused by pathogens or inflammatory bowel disease (IBD), can be assessed and monitored by examination of the levels of biomarkers such as calprotectin, lactoferrin, and lysozyme via this stool test. These markers can be used to differentiate between inflammation associated with potentially life-threatening inflammatory bowel disease (IBD), which requires lifelong treatment, and less severe inflammation that can be associated with irritable bowel syndrome (IBS) which is frequently due to the presence of enteroinvasive pathogens. Calprotectin and lactoferrin are only markedly elevated prior to and during the active phases of IBD, but not with IBS. Monitoring these levels in patients with IBD can therefore facilitate timely treatment of IBD, and can be ordered separately. Since the vast majority of secretory IgA (sIgA) is normally present in the GI tract, where it prevents binding of pathogens and antigens to the mucosal membrane, it is essential to know the status of sIgA in the gut. sIgA is the only bona fide marker of humoral immune status in the GI tract.
Cornerstones of good health include proper digestion of food, assimilation of nutrients, exclusion of pathogens and timely elimination of waste. To obtain benefits from food that is consumed, nutrients must be appropriately digested and then efficiently absorbed into portal circulation. Microbes, larger-sized particles of fiber, and undigested foodstuffs should remain within the intestinal lumen. Poor digestion and malabsorption of vital nutrients can contribute to degenerative diseases, compromised immune status and nutritional deficiencies. Impairment of the highly specific nutrient uptake processes, or compromised GI barrier function, as in "leaky gut syndrome," can result from a number of causes including:
- Low gastric acid production
- Chronic Maldigestion
- Food allergen impact on bowel absorptive surfaces
- Bacterial overgrowth or imbalances (dysbiosis)
- Pathogenic bacteria, yeast or parasites and related toxic irritants
- The use of NSAIDs and antibiotics